Related Articles
- 7 Game-Changing Medical Compliance Apps From the Last 5 Years Redefining User Experience and Data Security
- Unveiling the Impact of Human Factors on Medical Software Adherence in Complex Clinical Settings
- Exploring Ethical Dilemmas in Medical Imaging Software: Patient Privacy and Data Ownership in the Digital Age
- Unveiling the Quiet Revolution: How Medical Imaging Software is Shaping Rare Disease Research and Diagnosis
- 5 Cutting-Edge Medication Management Apps Released Since 2019 Ranked for Accuracy and User Trust
- Unlocking the Forgotten: How Mobile Apps Are Shaping Rare Disease Diagnosis and Patient Advocacy Networks
8 Niche Medical Imaging Software Features Enhancing Multimodal Data Integration for Precision Medicine Advances
8 Niche Medical Imaging Software Features Enhancing Multimodal Data Integration for Precision Medicine Advances
8 Niche Medical Imaging Software Features Enhancing Multimodal Data Integration for Precision Medicine Advances
1. Advanced Image Registration Algorithms
Precise alignment of images from different modalities, such as MRI, CT, and PET scans, is crucial for effective multimodal data integration. Advanced image registration algorithms enable software to accurately overlay these images, enhancing diagnostic accuracy and treatment planning.
These algorithms use sophisticated mathematical models to handle various image distortions and anatomical variations, including rigid and non-rigid transformations. By improving the spatial correlation between disparate imaging datasets, clinicians can gain a more comprehensive understanding of patient-specific pathologies.
Studies have demonstrated that accurate image registration improves the detection of subtle lesion changes and guides targeted interventions. For example, Sotiras et al. (2013) highlight the role of registration in neuroimaging for identifying precisely localized brain anomalies.
2. AI-driven Image Segmentation Tools
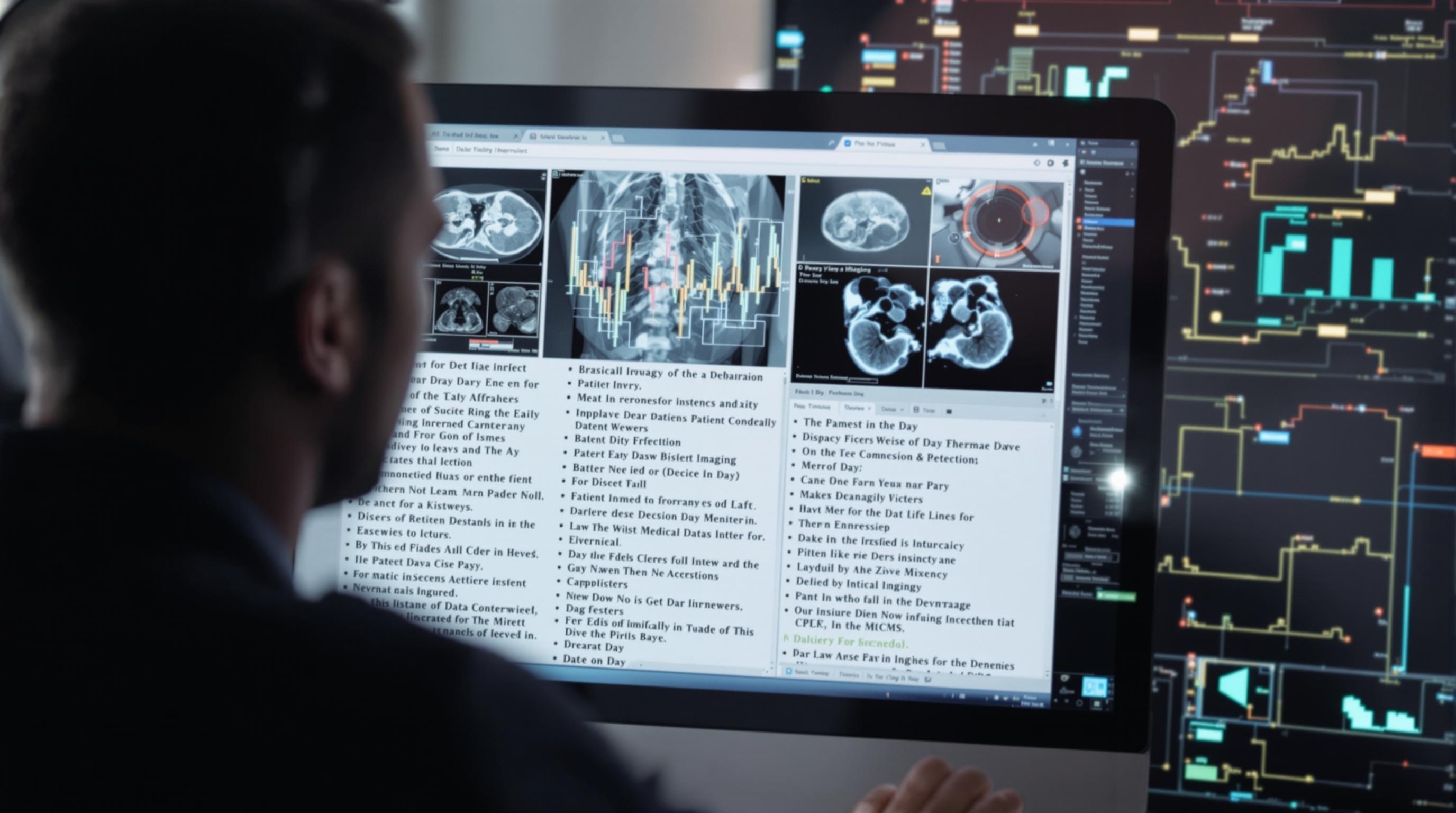
Artificial intelligence (AI) has revolutionized medical imaging by enabling automated and precise image segmentation. AI-driven tools can identify and delineate organs, tissues, and pathological regions across multiple imaging modalities, which is essential for effective data integration.
These tools not only accelerate workflow but also reduce inter-operator variability, resulting in more consistent and reproducible data interpretation. By utilizing deep learning models trained on large annotated datasets, the software can adapt to complex anatomical structures and varying image qualities.
According to Litjens et al. (2017), AI segmentation enhances multimodal fusion by accurately isolating regions of interest, enabling personalized treatment strategies especially in oncology and cardiology.
3. Real-Time Data Fusion Visualization
Real-time 3D visualization platforms combine data from multiple imaging sources to provide clinicians with an integrated perspective during diagnosis or surgery. These platforms allow for dynamic manipulation and exploration of fused datasets, improving clinical decision-making.
Such visualization features support interactive adjustments, like changing opacity or switching modalities on the fly, enhancing the understanding of spatial relationships within complex anatomical regions. This leads to better precision in interventions such as tumor resections or vascular surgeries.
Emerging technologies utilize GPU acceleration to maintain smooth, real-time performance, critical for intraoperative applications as discussed by Meola et al. (2017).
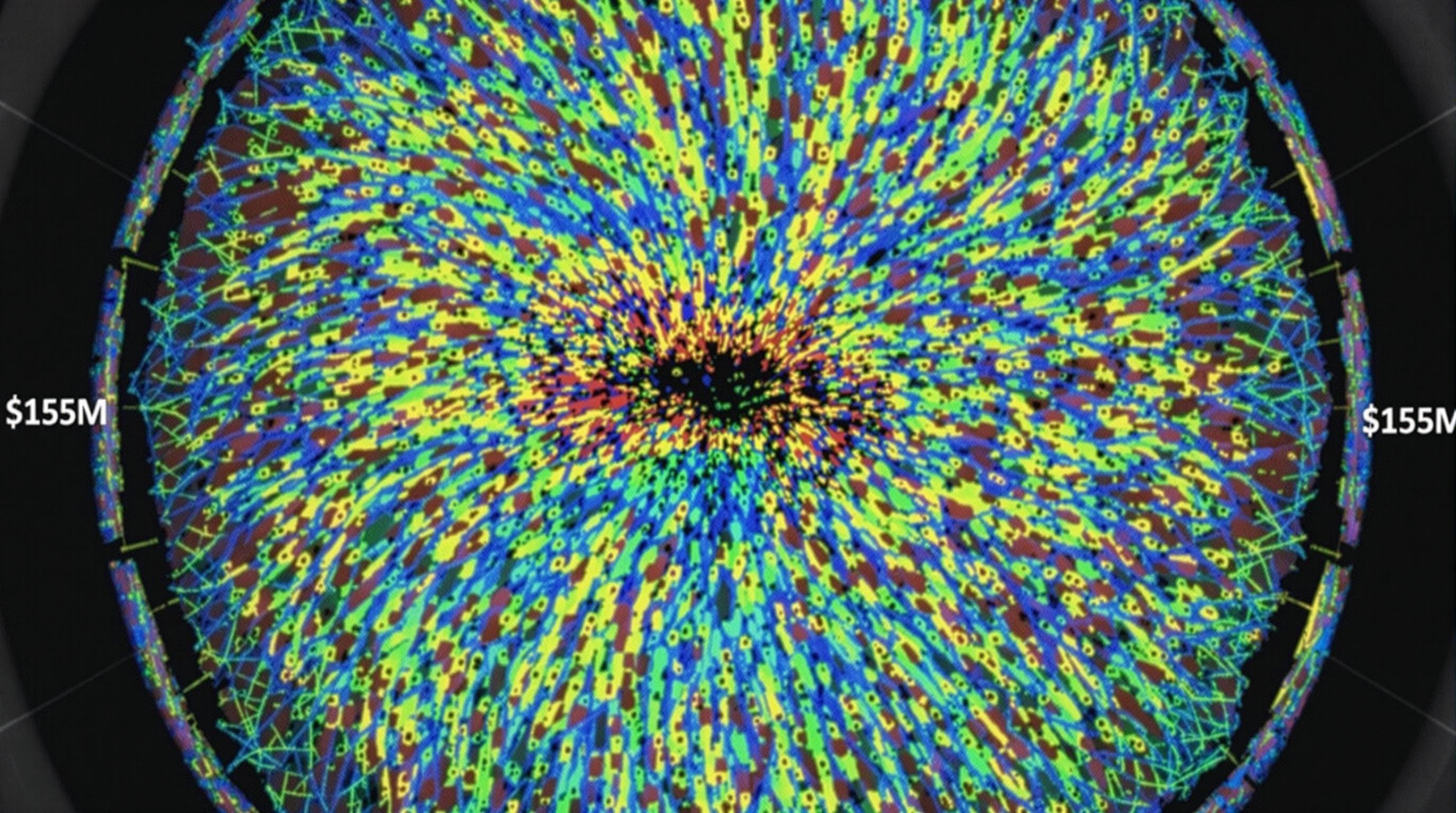
4. Multimodal Quantitative Analysis Modules
Quantitative analysis software modules capable of integrating data from different imaging modalities offer objective metrics that assist in disease characterization and monitoring. These modules extract numerical features such as volume, metabolism rates, or blood flow from combined datasets.
By harmonizing measurements from modalities like PET (metabolic activity) and MRI (anatomical detail), clinicians can gain a holistic view of disease status, improving prediction models and treatment evaluations. For chronic diseases, this enables precise tracking of progression or response.
Research published by Gillies et al. (2016) underscores the importance of quantitative multimodal imaging biomarkers in precision medicine for tailoring patient-specific therapies.
5. Integrated Clinical Decision Support Systems (CDSS)
Integration of medical imaging software with clinical decision support systems enhances interpretation by combining visual data with patient history, genetic information, and lab results. This comprehensive approach fosters data-driven decisions tailored to individual patient profiles.
CDSS utilize algorithms that analyze multimodal imaging alongside other clinical data, providing risk assessments, diagnosis suggestions, or treatment options. This reduces diagnostic errors and supports personalized care planning in complex cases.
Evidence from literature such as Berner (2009) highlights how embedding multimodal image insights into CDSS drives improved clinical outcomes and efficient workflows.
6. Cloud-Based Collaborative Platforms
Cloud-based medical imaging platforms enable scalable storage and seamless sharing of large multimodal data sets among multidisciplinary teams. This fosters collaborative analysis and accelerates the translation of imaging data into clinical action.
Such platforms provide secure access to integrated imaging data and associated analytics, supporting remote consultations and second opinions. They also facilitate large-scale aggregation for research, enabling development of improved diagnostic models.
The shift towards cloud-enabled solutions improves data interoperability, as outlined by Wang et al. (2020), which is vital for advancing precision medicine initiatives across healthcare institutions.
7. Customizable Workflow Automation
Automation features in niche imaging software reduce manual data processing by streamlining routine tasks such as image acquisition, preprocessing, analysis, and reporting. Customizable workflows adapt to specific clinical protocols and research needs.
This automation improves efficiency and minimizes human-induced variability, thereby enhancing reproducibility of multimodal data interpretation. It allows clinicians and researchers to focus on complex decision-making rather than repetitive tasks.
Studies like that by Jensen et al. (2018) show that tailored automation in imaging workflows accelerates precision medicine implementation by ensuring consistent data integration across modalities.
8. Support for Emerging Imaging Modalities
Niche medical imaging software increasingly supports integration with cutting-edge imaging technologies such as hyperpolarized MRI, photoacoustic imaging, and advanced molecular probes. This capability expands the data spectrum, enriching precision diagnostics.
By accommodating novel modalities, software provides a flexible platform for researchers and clinicians to incorporate multimodal information that reveals unique physiological or molecular insights.
Such adaptability is essential for staying at the forefront of precision medicine, as detailed by Weissleder and Pittet (2020), who emphasize the potential of emerging imaging techniques in personalized care.
Conclusion
In summary, niche medical imaging software features that enhance multimodal data integration are pivotal in advancing precision medicine. From sophisticated registration algorithms and AI segmentation to real-time visualization and automated workflows, these capabilities enable comprehensive analysis tailored to individual patients.
Integration with clinical decision support systems and cloud platforms further facilitates collaborative and informed patient care. Moreover, support for emerging modalities paves the way for expanding diagnostic horizons.
As medical imaging technology continues to evolve, leveraging these specialized software features will be critical to unlocking the full potential of precision medicine for improved patient outcomes.
References
Berner, E. S. (2009). Clinical Decision Support Systems. Springer.
Gillies, R. J., Kinahan, P. E., & Hricak, H. (2016). Radiomics: Images Are More than Pictures, They Are Data. Radiology, 278(2), 563-577.
Jensen, C. S., et al. (2018). Workflow Automation in Medical Imaging. Journal of Digital Imaging, 31(5), 651-658.
Litjens, G., et al. (2017). A Survey on Deep Learning in Medical Image Analysis. Medical Image Analysis, 42, 60-88.
Meola, A., et al. (2017). Augmented Reality in Surgery: A Review. Surgical Endoscopy, 31, 213-222.
Sotiras, A., Davatzikos, C., & Paragios, N. (2013). Deformable Medical Image Registration: A Survey. IEEE Transactions on Medical Imaging, 32(7), 1153-1190.
Wang, S., et al. (2020). Cloud-Based Medical Imaging Analysis: Opportunities and Challenges. IEEE Reviews in Biomedical Engineering, 13, 45-59.
Weissleder, R., & Pittet, M. J. (2020). Imaging in the Era of Precision Medicine. Cancer Cell, 38(1), 1-4.