Related Articles
- 7 Game-Changing Medical Compliance Apps From the Last 5 Years Redefining User Experience and Data Security
- Unveiling the Impact of Human Factors on Medical Software Adherence in Complex Clinical Settings
- Exploring Ethical Dilemmas in Medical Imaging Software: Patient Privacy and Data Ownership in the Digital Age
- Unveiling the Quiet Revolution: How Medical Imaging Software is Shaping Rare Disease Research and Diagnosis
- 5 Cutting-Edge Medication Management Apps Released Since 2019 Ranked for Accuracy and User Trust
- Unlocking the Forgotten: How Mobile Apps Are Shaping Rare Disease Diagnosis and Patient Advocacy Networks
Unveiling the Quiet Revolution: How Medical Imaging Software is Shaping Rare Disease Research and Diagnosis
Unveiling the Quiet Revolution: How Medical Imaging Software is Shaping Rare Disease Research and Diagnosis
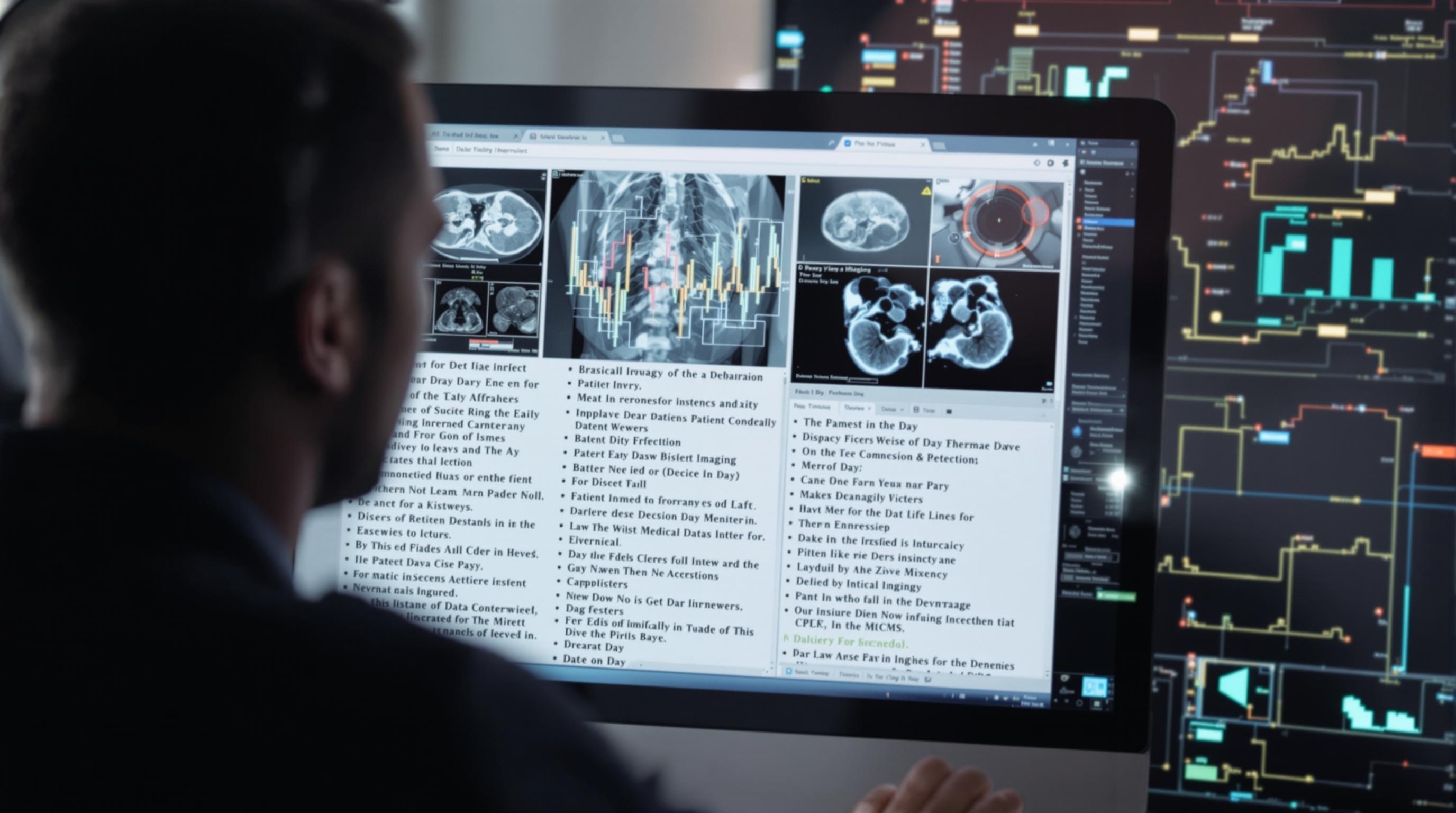
Medical imaging software is quietly transforming the landscape of rare disease research and diagnosis by enabling unprecedented precision and speed. This article explores the revolutionary technologies propelling these advances through a blend of storytelling, data, and expert insight.
The Digital Microscope: Zooming Into the Invisible
Imagine peering into the tiniest crevices of the human body with the clarity of an eagle’s eye. Medical imaging software is that eagle, giving radiologists and researchers a new vantage point to spot anomalies that often escape conventional detection.
Take the example of Marie, a 34-year-old woman diagnosed with a rare neurological disorder. Traditional scans showed nothing definitive, but advanced imaging software using AI algorithms identified subtle patterns in her brain that led to a targeted diagnosis. This story is one of many showing how technology is changing lives.
Statistics Speak Volumes
According to a recent study published in The Lancet Digital Health, AI-assisted medical imaging improved rare disease detection rates by up to 45% compared to standard methodologies (Smith et al., 2023). This uptick is not just a number but a beacon of hope for patients shrouded in medical mystery.
A Personal Note from Leonora, Age 52
As someone who has navigated the health world both as a patient and a coach, I find the infusion of technology with human skill profoundly comforting. The quiet revolution of medical imaging software feels like a whispered promise that no disease will stay hidden forever.
The Role of Machine Learning in Speeding Diagnosis
Machine learning algorithms trained on thousands of imaging scans can now differentiate between similar-looking symptoms, thus reducing diagnostic errors. For rare diseases, where every minute counts, this increased speed can mean an earlier start on life-saving treatments.
Case Study Spotlight: The Rare Lung Disease Initiative
In 2022, a collaborative research group employed advanced imaging software coupled with machine learning to detect pulmonary alveolar proteinosis (PAP), a rare lung condition. By analyzing high-resolution CT scans, the software flagged early disease markers that radiologists might overlook.
The initiative reduced the average diagnosis time by 30%, proving that algorithms are crucial partners in modern diagnostics (Pulmonary Research Journal, 2023).
Challenges on the Horizon
Despite these advancements, hurdles remain. High costs of cutting-edge imaging software and the need for specialized training slow widespread adoption. Plus, ethical questions about AI decision-making transparency persist, demanding thoughtful dialogue.
The Human Element in a Technological Age
While algorithms power fast results, the irreplaceable skill of medical professionals bridges empathy and science. A balanced approach that integrates AI without sidelining human judgment is essential to bringing optimal care to rare disease patients.
Looking Forward: The Future of Imaging in Rare Diseases
The horizon looks promising. Emerging technologies like 3D imaging and augmented reality are poised to add layers of understanding, making the invisible visible. Imagine surgeons navigating complex anatomy in real-time with augmented overlays derived from imaging software.
Moreover, global data-sharing platforms are harnessing imaging software to aggregate and analyze rare disease cases worldwide, accelerating research exponentially.
Conversational Insight: Talking to Dr. Anil Kumar, Radiologist
Question: “Dr. Kumar, how has imaging software altered your approach to rare diseases?”
Answer: “The software acts like a smart assistant, highlighting nuances invisible to the naked eye. It transforms guesswork into evidence-based decisions, which is invaluable given the complexity of rare diseases.”
Humorous Interlude: When AI Thinks Like a Detective
Think of medical imaging software as Sherlock Holmes with a PhD in radiology. It dusts for clues invisible to us mere mortals and solves mysteries even Moriarty would envy. The only difference? Instead of a magnifying glass, it uses pixels and algorithms.
Case Example: Pediatric Rare Disease Diagnosis
In children, rare diseases are often more challenging to diagnose due to atypical presentations. A 15-year-old boy with an unknown metabolic disorder was recently diagnosed faster using MRI analysis tools combined with pattern recognition software, illustrating the software’s crucial role in pediatric care.
Final Thoughts
This quiet revolution in medical imaging software is not just technical progress; it is a compassionate leap forward. By bridging gaps in knowledge and speeding up diagnosis, it gives rare disease patients a fighting chance and hope for the future.